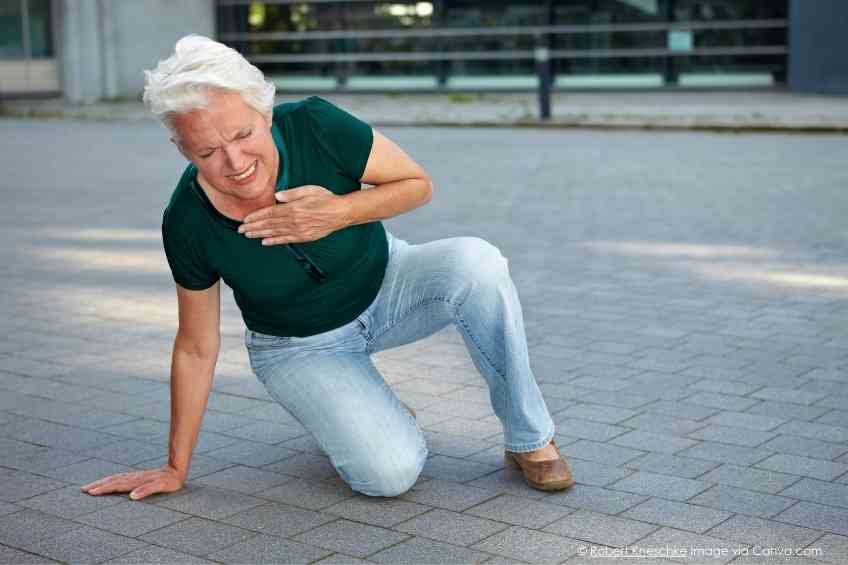
There is an almost secret killer praying on women that is taking thousands of lives every year in the United States. The culprit is cardiovascular disease, a threat that tradition tells us is more of a danger to men than women. Unfortunately, heart disease is an equal opportunity killer. It is the leading cause of death for both men and women. What’s perhaps more troubling is that after years of success in battling back this deadly disease, the threat has been growing again in recent years—putting women in more danger than ever. Thankfully, Dr Harmony Reynolds recently spoke to WellWell on why this is happening, the remedies and how the American Heart Association is leading the fight to educate women on how to take charge of battling back. Read on.
Cardiovascular disease is reputed to be the leading cause of death among men and women. The perception is that men suffer more than women. Is that accurate?
Heart disease is the leading killer of women and this is true around the world affecting every race and ethnic group. So yes, I agree with you, there’s been this public perception that this is not a problem for women and that’s just wrong.
Why is that perception out there?
Women tend to get heart disease on average later than men. Maybe about 10 years later and maybe that’s the reason, I’m not sure. But, back in the day, the American Heart Association put out a handbook about heart attacks for women. And it’s if your husband has a heart attack, here’s what you do. Now we’ve come a long way since then. The American Heart Association is now leading in trying to get this message out to women, but sometimes these old ideas stick.
Cardiovascular disease seems to be a growing threat to everyone. Is the risk growing for women?
It is and unfortunately, it’s growing for men as well. We have seen a long decline in the number of cardiovascular deaths in men and women over maybe 50 years and in the last three or four that rate is going up again.
And why is that? Is it a dietary or weight issue or is it a combination of things?
I think that it’s a set of cardiovascular risk factors that are again on the rise. The long-term trend that was downward had to do with less smoking, a better diet overall, better access to care and a general understanding of risk factors even if they weren’t being controlled as well. I think people were starting to get the message, but lately, as you said, we’ve seen a huge rise in obesity and the accompanying risk factors related to obesity. Plus, pregnancy complications are on the rise and that might be something related to heart disease in women over the long run. For whatever reason, the number of deaths and cardiovascular disease is going up, and that’s an emergency, in my view.
Fewer people are smoking, so that should have somewhat of a counterbalancing impact. Is that correct?
Thank goodness fewer people are smoking now. We’re seeing vaping as a problem, and that’s something that we need to nip in the bud, especially in the younger population. But thank goodness smoking is on the decline because smoking is the biggest risk factor when it’s present.
Do we see the problem growing at a faster rate in the U.S. or is it growing worldwide at the same rate?
The worldwide numbers are outpacing even the United States. There’s been just an explosion of cardiovascular deaths worldwide, probably because we’re getting towards defeating some of the communicable diseases and that leaves us vulnerable to cardiovascular disease. I saw a statistic that there had been 2,000,000 deaths from cardiovascular disease in the world 20 years ago, and now we’re at 9 million. There’s more of a shift towards a Western unhealthy diet towards less exercise and thankfully we’re having fewer deaths from, let’s say, bacterial disease because antibiotics are more available. But then as people survive, if they don’t have healthy habits, they’re vulnerable to heart disease.
Is the risk greater for women? Does it differ among ethnic groups? Are there subgroups that are at even greater risk of heart disease or of seeing a disproportionate rise in cardiovascular issues?
Yes, we’re seeing a disproportionate rise in women from underrepresented racial minorities like black and Latino women. And I think that probably parallels a rise in risk factors among these women, especially obesity and hypertension.
Why is the risk rising for pregnant women or new moms?
We’re trying to shine a light on what happens in a pregnancy can reveal a lot about cardiovascular risk. There are adverse pregnancy outcomes as they’re now called, and they range from high blood sugar, that gets called gestational diabetes, high blood sugar and pregnancy or high blood pressure in pregnancy. High blood pressure and pregnancy might be because there was a pre-existing high blood pressure problem or a new high blood pressure problem during the pregnancy. If it gets bad towards the end and there are associated findings, let’s say with the kidneys or the blood counts, we call that pre-eclampsia. Even having a small baby is considered an adverse pregnancy outcome or delivering early and all these things are associated with a higher risk of cardiovascular disease, not just immediately, but for the woman’s entire lifetime. And that risk persists 10-20 years down the line. Now this is a big problem because women often get lost in care. In that time frame, after delivery, they tend to go to their obstetrician and think about that aspect of their health. But they don’t necessarily check in about general health. And certainly, heart health. So, we miss an opportunity for prevention there. One of the key messages that we want to get out is that women need preventive care because heart disease is preventable and treatable.
You’re involved with the AHA’s Go Red for Women, which is a program designed to raise awareness for cardiovascular disease among women. Are women more aware of cardiovascular risks?
Yes and no. I would like to say that this is a definite win for the Heart Association, the CDC and the NIH, but we’re seeing that we’re getting losses actually in knowledge over time. The initial push converted a lot of women to the understanding that heart disease is a huge health threat. But for some reason that messaging has not gotten through in a sustained way, and I’m not sure if that means we need to reach people in new ways. In recent years, the American Heart Association has conducted periodic surveys of random women just to see what the understanding is about heart disease, about risk factors and about what you can do. And in the last 10 years, there’s been a huge decline in the understanding of heart disease as the leading killer. The worst knowledge losses are in the people who are most at risk, our underrepresented women, black women, Latino women and young women. And that worries me for the future because we can do so much for prevention from an early age, a healthy diet that sticks with us, a healthy lifestyle, healthy exercise and knowing your numbers. And if people don’t recognize heart disease as a threat, then it’s a lot harder to think that we’re going to do something about it.
With so much information out there about heart disease, why do you think that’s happening, that loss of awareness?
I don’t know. I’m not sure if people are just getting their information from different sources. I’m not sure what to think about it. It’s sort of become if you know, you know. There’s sort of an echo chamber of people who know this and keep saying the same information over and over, but we just need new channels.
How much of this awareness do you think falls on the medical community? There seems to be a connection to doctors not raising awareness during annual checkups.
I agree with you. I think there have been huge advances in doctors being proactive about risk factors among women, but we still have a problem that every woman gets a chat with her doctor about the need for a mammogram or a pap smear. And I’m not hearing that every woman is being told your blood pressure is high. I’m hearing borderline cholesterol. It’s for preventive care, but I’m not hearing what I think we should be hearing. which is your blood pressure is high and we need to treat it. I’m an outpatient cardiologist and you know office cardiology is hugely impactful, but sometimes the folks who are in the hospital and dealing with the patients who are at death’s door sort of got the corner on the market of reducing the risk of cardiovascular death. But in reality, in the office, if you lower somebody’s blood pressure by 10 points and then you sustain that for 10 years, you save a life.
Emergency room care is more likely to assume a man has a heart attack than a woman when they come in with the same symptoms. What do you think of this?
One of those studies is actually from our group, showing that young women who came to the emergency department with chest pain waited on average 11 minutes longer than young men and black women waited another 10 minutes and time is myocardium, we say in the cardiology business. The longer you wait with a heart attack, the more likely there is to be permanent damage. If somebody’s having chest pain and might be having a heart attack, I’m very concerned that fewer women are being seen by specialists. Fewer women were being admitted for observation of their chest pain in this large ER study. And there are many similar studies showing that there is a bit of a difference. There’s a disparity in care for women. And that’s why when I counsel my patients about when they come into the emergency room, to say I think I’m having a heart attack because you want to focus the physician on the concern.
How do we change the focus of a segment of the medical community?
Women need to advocate for themselves. Women need to be educated about how to take better care of themselves and exactly what the risk factors are, why this is important for them and what they can do. I certainly don’t mean to malign emergency room doctors who are working super hard and generally doing a great job. But, I’ve heard a bunch of horror stories about the people who went to doctors who weren’t up to speed and weren’t doing exactly what they might need to do. So that’s why I tell my women to be very specific and ask questions. It can’t hurt and it might help.
What do women need to do to maintain heart health, recognize symptoms and proactively address these challenges?
There are two big things that we need to talk about in relation to that question. One of them is the symptoms of heart attack, which is typically going to come with chest pain. But the pain might not be painful. It might just be a discomfort. Every patient of mine said I thought that the heart attack would be so bad that I wouldn’t be able to stand it and because she could stand it, she thought that wasn’t it. And she was late in coming in and suffered some damage. So, heart attack pain doesn’t have to be so bad that you can’t stand it. It might just be uncomfortable, and it will generally be in the chest, but it might be outside the chest. It might be in the jaw, the neck, shoulders, arms, back, upper stomach or in the chest. It might be all of those places or just a few of them. It might be accompanied by shortness of breath, nausea, vomiting, sweating or a sense that something is terribly wrong. It could be only those things you don’t have to have chest discomfort. But in general, women will have chest discomfort and often one or another symptom as well. And if you’re not sure, it’s best to come in. If you’ve had 10 minutes of a symptom, call 911 because that’s how you get the most expedited treatment. People who decide they’re going to drive themselves run the risk of hurting somebody on the road if they’re having a heart attack. And they’re not going to get the same expedited treatment because people generally take you more seriously if you come in by ambulance. And whenever I tell people that long list of symptoms that might be a heart attack, they tend to get concerned because almost everybody’s had one of those things in the last couple of months. And I’ll say, all right, if you have the sausage and pepper hero and you’ve got some terrible heartburn after, well, you know what that is? If you’ve had it before, and next time you have it, you’re not going to suddenly think it’s a heart attack just because you know that heartburn can be a heart symptom. But if you’re feeling something that you’re not familiar with or it’s in a position that doesn’t seem like what you’d expect, then you need to call 911 if that symptom is going on for 10 minutes or more.
What are the critical things women can do proactively to maintain good heart health?
The American Heart Association has a framework called Life Essential 8. If you’re a smoker, every single cigarette you choose not to pick up, reduces your risk, and this is from a worldwide study. It’s exactly true that 6 cigarettes are less risky than seven is less risky than eight, and one is better and none, of course, is the goal. So, no smoking. And no nicotine products at all and try not to inhale any smoke of any kind.
Next cholesterol. We want low blood cholesterol because cholesterol is the main component of plaque that blocks arteries and causes a heart attack and something that people don’t always know is that plaque of any size can break and cause a heart attack. The analogy I like to use is it’s a lot like a raw egg. It’s got a thin shell and a bunch of gooey stuff inside, and if the shell breaks, because eggs are fragile, then the stuff oozes out and it makes a big mess. So, in this case, the flowing blood will contact the interior of that plaque and a blood clot will form. That’s what causes a heart attack and stroke. That does not need to be an artery that was badly blocked beforehand. And stress tests are only meant to find 80-85 percent narrowing or more. So, you could have a stress test one day and have a quiet plaque that’s let’s say, 40 percent narrowing. And the next day, if that plaque decides to act up, that person could have a heart attack. A stress test is not going to be a good indicator. When we lower cholesterol a lot and we manage all the risk factors. How do we lower blood cholesterol? Mostly by lowering saturated fat in the diet and saturated fat is in a lot of different foods. It’s in red meats, butter, cheese, desserts, baked goods, fried foods, chips, sausage and coconut oil. Read the food label and if it’s high in saturated fat try and find a replacement.
The next one is blood pressure. A normal blood pressure is 115/75. If your blood pressure is over 130 for the top number, the systolic when the heart beats or over 85 for the bottom number in between beats, and certainly if it’s over 140/90, you’re going to want medication for that lifestyle. Measures that can be effective are reducing salt and increasing exercise. Generally eating more fiber and more vegetables may be healthy, but you’ve got to know your numbers and don’t be so quick to discount a high blood pressure. Because if blood pressure continues to be high, you really should get treated.
Next is healthy weight. It’s useful to check your body mass index, which is just an index of weight to height. It’s available online. We want that to be less than 25. We are looking for 20 minutes of at least moderate intensity exercise every day. At least six days a week. The more exercise, the better. So, if you can’t get to 20 minutes because you can’t get to a gym, no problem, just get up. Go walking for 5 minutes, put a song on dance for 5 minutes and dance to one song or two songs. Every little bit you do counts, and I recently learned that something that’s called VILPA (vigorous intermittent lifestyle physical activity) is also very protective. Like walking up the stairs to get something on the 2nd floor or in a city, running up the subway stairs or running down one block. Jog to catch the bus. Those little bits, like exercise snacks, are also protective and that’s separate from the moderate stuff.
Are there any other issues or challenges that aren’t apparent in helping women?
I think a huge challenge is the availability of healthy food. There are many food deserts. It can be hard to get great vegetables. It can be hard to get great fish. I think that we need to change through public policy. But for now, I’m happy to know that there are food pantries available and they often have fresh vegetables. And also, people sense a lack of time when thinking about the preparation of vegetables. But microwaveable vegetables are great. I get boxed microwave vegetables to have with my family during the week because like many of your readers, I’m busy and it can be hard to prep things. But frozen vegetables have the nutrients that we’re looking for. And it’s fine to pop them in the microwave and make sure you get a serving during the day. I think easy healthy snacks are not as widely available as I would like and that makes it tough for people on the go. There are also tons of misinformation. You just really want to try and get good quality information.
Are there other misconceptions out there that people just need to become aware of?
I think there are a couple of important things I mentioned about stress testing. I think people have the sense that if they pass the stress test they’ve got a clean bill of health. And unfortunately, that’s just not so. Another big misconception is that women’s symptoms are different. I think we’ve done a very good job of conveying the idea that a woman’s symptoms don’t have to be classic textbook, exactly like a man’s. People expect a heart attack to feel like it looks in the movies on men and for women, it really may not be that way. Another misconception is that heart disease in women needs to look exactly like it looks in men. There is definitely the type of blocked artery, heart disease in women that there is in men. There’s congestive heart failure can be very similar in women than men. But there can be some differences. There’s a whole set of problems that are caused by things other than blocked arteries like small artery disease or artery spasms that cause true cardiac chest pain in women. So that worries me because I think some people get a pat on the head and get told, oh, you’re fine.
 About Harmony Reynolds, MD
About Harmony Reynolds, MD
Dr. Harmony Reynolds is a cardiologist and director of New York University Langone’s Sarah Ross Soter Center for Women’s Cardiovascular Research, working closely in support of the American Heart Association. She is also an associate professor in the Department of Medicine at NYU Grossman School of Medicine in New York City. Her special interest and clinical and research focus are heart disease in women, its causes and treatments.
Please visit the American Heart Association to learn more.