By Sean Zucker –
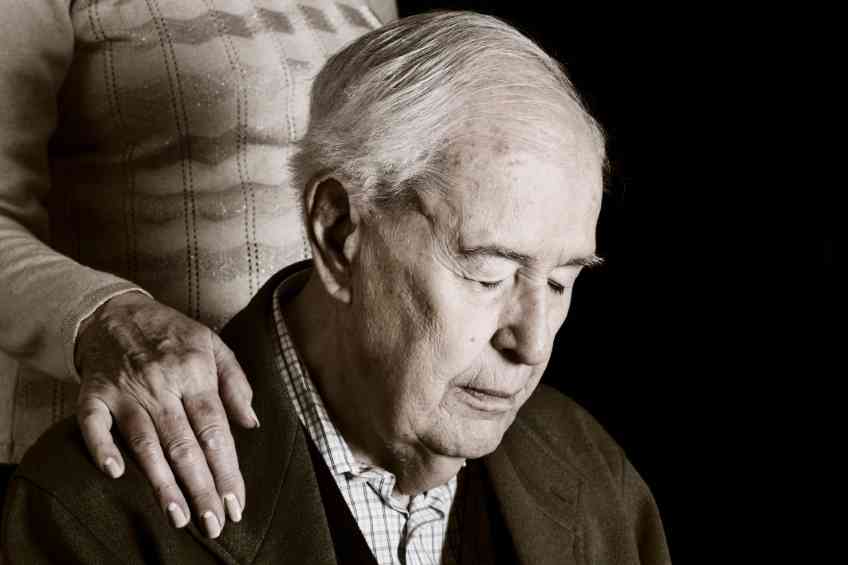
Alzheimer’s is a painfully debilitating and impactful disease. Worse yet, it’s widespread. The Centers for Disease Control and Prevention (CDC) reports nearly six million Americans are now living with Alzheimer’s, which makes it the most common form of dementia.
It is not only debilitating, but it is also deadly. It’s the fifth leading cause of death in America. It is also growing. The number of people afflicted is projected to nearly triple to 14 million by 2060. These depressing numbers and projections welcome any positive advancements in Alzheimer’s Disease treatment or early detection. One new study offers significant hope for early detection by noting that the initial signs of Alzheimer’s may appear in the eyes.
Researchers at Cedars-Sinai in Los Angeles concluded after analyzing tissue from the retinas and brains of 86 donors with varying degrees of mental decline. The team then compared those samples with tissue from donors with normal cognitive function.
“Our study is the first to provide in-depth analyses of the protein profiles and the molecular, cellular and structural effects of Alzheimer’s disease in the human retina and how they correspond with changes in the brain and cognitive function,” the study’s senior author Dr. Maya Koronyo-Hamaoui said.
The team focused on retinas due to their function as the light-sensitive layers of nerve tissue in the back of the eye. Their positioning makes them crucial to understanding Alzheimer’s possible earliest symptoms. “The retina, a developmental extension of the brain, offers an unparalleled opportunity for affordable, noninvasive monitoring of the central nervous system,” added Yosef Koronyo, a research associate at the Cedars-Sinai. “And with the help of our collaborators, we discovered the accumulation of highly toxic proteins in the retinas of patients with Alzheimer’s disease and mild cognitive impairment, causing severe degeneration of cells.”
The Cedars-Sinai analyzed the proteins present in both the retina and brain tissues and ultimately found an excess amount of amyloid beta 42, a protein that in the brains of Alzheimer’s patients causes the plaques that disrupt cognitive function. This protein was also discovered in the cells that bridge visual input from the retina to the optic nerve.
“These changes in the retina correlated with changes in parts of the brain called the entorhinal and temporal cortices, a hub for memory, navigation and the perception of time,” Koronyo-Hamaoui explained.
The insights are more than simply intriguing. They may help develop new ways to treat the disease in its early stages before extensive damage takes place. Without reliable, systematic detection methods, the early stages of Alzheimer’s are usually identified by symptoms such as increasing and episodic memory loss, trouble handling money or bills, difficulty completing familiar tasks and decreasing judgment. The work by Cedars-Sinai may help change this diagnostic approach.
“Because these changes correspond with changes in the brain and can be detected in the earliest stages of impairment, they may lead us to new diagnostics for Alzheimer’s disease and a means to evaluate new forms of treatment,” noted Dr. Keith Black, the study’s co-author and chair of the Department of Neurosurgery at Cedars-Sinai.